
VERTIGO
647-425-4669
Trigeminal Neuralgia
Trigeminal neuralgia (TN) is a painful condition affecting the major nerve of the face, often described as sudden, electric-shock-like pain. In this blog, we’ll explore what causes it, common symptoms, and how physiotherapy can play a powerful role in relief—by addressing the jaw, neck, tongue posture, and calming nerve sensitivity through treatments like acupuncture, desensitization, and gentle exercises.
What is Trigeminal Neuralgia?
Trigeminal neuralgia is often described as one of the most intense pain conditions a person can experience. If you’ve ever felt sudden, electric-shock–like pain on one side of your face, you may understand how disruptive and distressing it can be. Fortunately, there are ways to manage it—and physiotherapy can play an important role in reducing symptoms and improving quality of life.
Trigeminal neuralgia is a chronic pain disorder that affects the trigeminal nerve, the main sensory nerve of the face. You may experience episodes of severe, stabbing, or burning pain, typically on one side of your face. The pain often comes in short bursts that can last from a few seconds to a few minutes, and may be triggered by everyday activities such as talking, eating, brushing teeth, or even a light touch on the cheek.
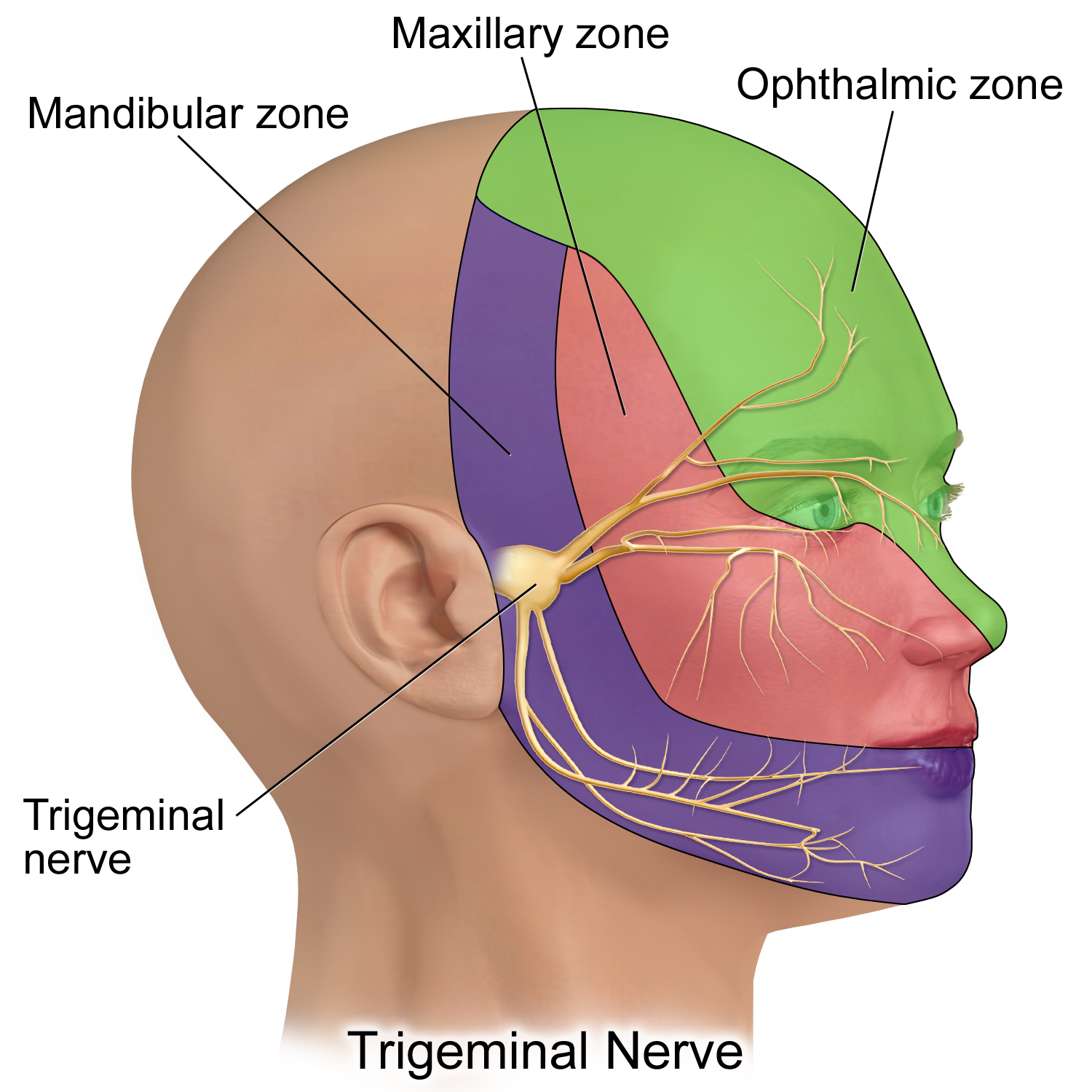
Anatomy of the Trigeminal Nerve
To understand trigeminal neuralgia, it helps to know a little about the trigeminal nerve itself. The trigeminal nerve (cranial nerve V) is the largest cranial nerve. It has three main branches:
Ophthalmic: sensation from the scalp, forehead, and upper eyelid.
Maxillary: sensation from the cheek, upper lip, upper teeth, and side of the nose.
Mandibular: sensation from the jaw, lower teeth, lower lip, and also motor function for chewing muscles.
Because this nerve carries sensation from so much of the face—and connects with muscles that control chewing—it can easily be influenced by both jaw and neck mechanics.
What Causes Trigeminal Neuralgia?
The exact cause of TN can vary from person to person, but the condition usually happens when the trigeminal nerve becomes irritated or compressed. Common causes include:
Blood vessel compression: The most frequent cause is when a blood vessel presses against the trigeminal nerve near its root at the brainstem. This constant pressure can wear away the protective coating around the nerve (called myelin), making it more sensitive and prone to firing off pain signals.
Multiple sclerosis (MS): In some cases, TN is linked to MS, a condition that damages myelin in the nervous system.
Tumors or structural changes: Rarely, a tumor or other growth can press on the trigeminal nerve.
Post-traumatic or dental causes: Facial injury, dental procedures, or jaw dysfunction may irritate the trigeminal system.
Idiopathic (unknown): Sometimes no clear structural cause is found, but the nerve is still hypersensitive.
While these are the “medical” causes, it’s also important to recognize that jaw and neck mechanics can contribute to irritation. Tension in the temporomandibular joint (TMJ) or stiffness in the cervical spine can increase strain on the trigeminal system, worsening symptoms or triggering attacks.
Symptoms
The main feature of trigeminal neuralgia is sudden, severe facial pain. People often describe it as:
Sharp, stabbing, or electric-shock pain that is deep on one side of the face. It typically increases in less than 20 seconds and may fade away within seconds to minutes. The excrutiating pain can cause you to grimace or wince.
Pain that comes in bursts lasting seconds to a few minutes, often repeating in cycles.
Trigger-sensitive pain—everyday activities like eating, drinking, brushing teeth, talking, shaving, putting on makeup or even a light breeze on the face can set off an attack.
Pain localized to areas supplied by the trigeminal nerve, such as the jaw, cheek, teeth, gums, lips, or around the eye.
Periods of remission and flare-ups—symptoms may disappear for weeks or months, then return.
Over time, some people may also experience a dull, aching or burning background pain between sharp episodes.
These symptoms can be frightening and exhausting, often affecting quality of life, mood, and confidence in daily activities. Recognizing the symptom pattern is an important step toward getting the right diagnosis and treatment.
Involvement of the TMJ and Cervical Spine
The trigeminal nerve doesn’t work in isolation. It has important anatomical and functional connections to the temporomandibular joint (TMJ), the upper cervical spine and even the tongue.
The mandibular branch supplies sensation to the jaw and also controls the chewing muscles. When the TMJ is tight, inflamed, or out of alignment, it can irritate this nerve branch, leading to worsening facial pain or triggering flare-ups during activities like chewing or talking.
The trigeminal nerve also shares pathways with the upper cervical spinal nerves (C1–C3) in a region called the trigeminocervical nucleus. This overlap means that problems in the neck—such as stiffness, poor posture, or muscle tension—can “feed into” the trigeminal system and amplify facial pain.
This is why many people with trigeminal neuralgia also notice symptoms in their jaw or neck, and why physiotherapy that addresses these areas can make such a difference.
How is Trigeminal Neuralgia Diagnosed?
Diagnosis is usually based on a person’s medical history. Your heathcare provider may:
Take a detailed history of your pain pattern and triggers.
Use imaging (MRI or CT scan) to rule out causes such as vascular compression, multiple sclerosis, or tumors.
The International Headache Society (IHS) has published specific criteria for Trigeminal Neuralgia:
A) Paraxysmal attacks of pain lasting from a fraction of a second to 2 minutes, affecting 1 or more divisions of the trigeminal nerve and fulfilling criteria B and C
B) Pain has at least 1 of the following characteristics:
Intense, sharp, superficial or stabbing
precipitated from trigger areas or by trigger factors
C) Attacks seterotypes in the individual patient
D) No clinically evident neurological deficit
E) Not attributed to another disorder
The hallmark sign is brief, intense, electric-shock facial pain triggered by light touch or routine activities.
How Can Physiotherapy Help?
While medication or surgical interventions are often discussed in trigeminal neuralgia treatment, physiotherapy offers a conservative and highly individualized approach that addresses the musculoskeletal factors contributing to nerve irritation.
Treatment may include:
Manual therapy: gentle mobilizations of the neck, upper cervical spine, and TMJ to reduce joint stiffness and improve alignment.
Soft tissue release: easing muscle tension in the jaw, face, and neck that may contribute to compression or sensitivity of the trigeminal nerve.
Posture retraining: correcting head, neck, tongue and jaw positioning to reduce strain on both the TMJ and cervical spine.
Jaw relaxation strategies: exercises to reduce clenching or grinding habits.
Acupuncture: targeted needling techniques can help calm irritated nerve pathways, reduce facial and jaw muscle tension, and improve the body’s natural pain-relief response.
Desensitization techniques: gradual, gentle stimulation of the affected areas (using touch, temperature, or texture) to help retrain the nerve and reduce hypersensitivity over time.
Neurodynamics (nerve glides): specific exercises to gently mobilize the trigeminal nerve and help restore normal movement and sensitivity.
By improving the way the jaw and neck move and interact with the trigeminal system, physiotherapy can help calm nerve irritation and reduce pain intensity and frequency.
Trigeminal Nerve Stretch
One useful exercise is the trigeminal nerve stretch (sometimes called a neural mobilization or glide). This should always be taught by a trained clinician, such as the therapists at Healing Vertigo, to ensure it’s appropriate for your condition.
Here’s a simple version:
Sit upright with good posture.
Tuck your chin so you create a “double chin”
From here, tilt your head away from the side you are treating.
Then gently turn your nose down towards the ground.
To stretch the mandibular branch, shift your jaw side to side.
To stretch the ophthalmic branch, shift your eyes side to side.
You may feel a gentle pulling or stretch along the jaw, cheek, or temple area—this should never be painful, only a mild stretch.
This exercise works best when combined with other strategies that improve TMJ function and cervical spine mobility.
Take Away Points
Trigeminal neuralgia can feel overwhelming, but you are not without options. A comprehensive approach—including medical management and physiotherapy that looks closely at the TMJ and cervical spine—can help reduce pain, restore function, and improve quality of life.
If you are struggling with facial pain or have been diagnosed with trigeminal neuralgia, a personalized physiotherapy program may help you find relief. To learn more about how the therapists at Healing Vertigo can help, book a free consultation now or send us an email at cheryl@healingvertigo.com
TN Treatment Near Me
If you are struggling with facial pain or have been diagnosed with trigeminal neuralgia, a personalized physiotherapy program may help you find relief. Book an assessment today or reach out with questions—we’re here to help you feel better and supported again.
Disclaimer: This advice is not meant to be a substitute for advice from a medical professional regarding diagnosis, prognosis, or treatment. Always seek advice from your physician, physiotherapist, or other qualified healthcare provider with questions you may have regarding a healthcare condition. The information of this website and email, including but not limiting to text, graphics, videos, images, and other materials are for informational purposes only. Reliance on the information on this website and email is soley at your own risk.